In case you’re not familiar, diabetes is a condition where your body either doesn’t produce enough insulin or can’t effectively use the insulin it does produce. This leads to high blood sugar levels, which can cause many of health problems if left unchecked. This includes your eyes.
Unfortunately, many of the most common diabetic eye diseases aren’t reversible, including diabetic retinopathy and diabetic macular edema. But don’t lose heart! There’s still plenty we can do to help manage the situation and protect your remaining vision.
Diabetes & Your Eyes
Diabetes is a chronic disease that affects millions of people. Roughly 90% of people with diabetes have type 2, which usually develops in adults. But whether we’re talking about type 1 or type 2, they both affect how your body produces or uses insulin. Insulin is vital for regulating sugar, or glucose, in our blood.
Symptoms of diabetes can include:
- Increased thirst
- Frequent urination
- Changes in weight
- Slow-healing injuries
- Fatigue
- Blurry vision
- Double vision
- Tingling or numbness in hands or feet
Since diabetes affects your blood vessels, it can be particularly harsh on your eyes and, more specifically, your retina.
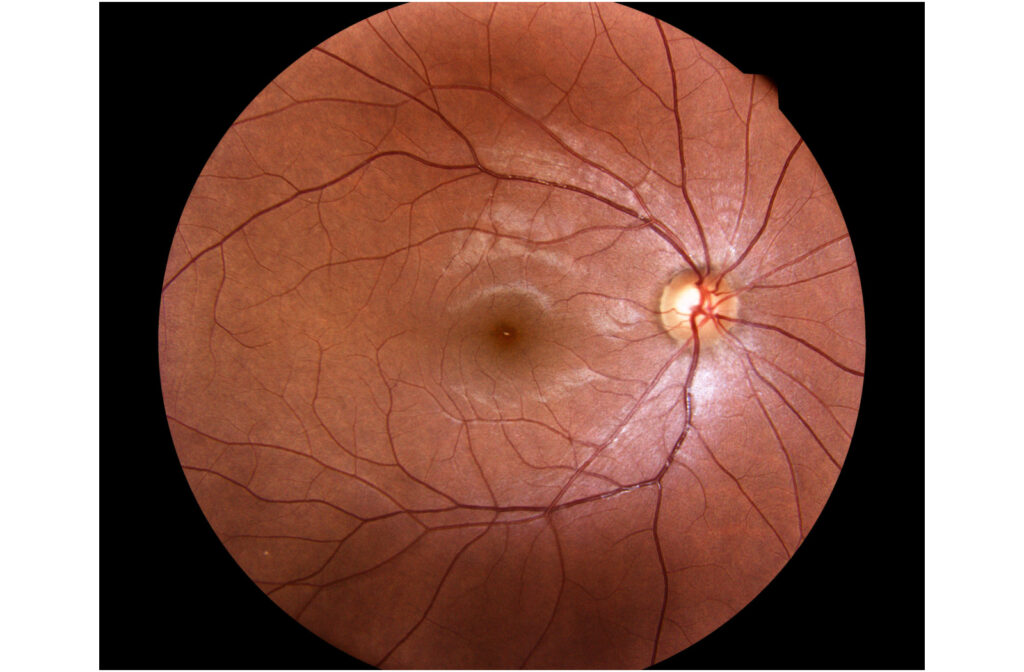
The retina is a layer of photoreactive cells sitting at the back of the eye. When light strikes the retina, it sends that data to the brain, where it’s decoded into an image. The retina is also one of the only parts of our body where we can directly observe blood vessels at work. During a comprehensive eye exam, we can use this as a window into your health,
What is Diabetic Retinopathy?
Many people with diabetes also have some form of diabetic retinopathy, making it the leading cause of blindness in working-age adults.
As we mentioned, diabetes causes your blood sugar levels to fluctuate. These fluctuations can be extreme and can eventually damage the tiny blood vessels in the retina, which causes them to swell, leak, and bleed into the retina, affecting your vision.
During the “proliferative stage,” your eye could try to compensate for the damaged blood vessels by growing new ones. Unfortunately, these new blood vessels are weaker, so they also rupture and leak into the eye.
Sometimes, you may not notice any changes to your vision until the disease has advanced and the damage is already occurring. This is what makes routine eye exams so important. Eventually, you may notice:
- Blurred vision
- An increase of floaters in your vision, including red floaters
- Distorted vision, such as straight lines appearing wavy
- Sudden vision loss
We can observe these changes in the retina during your eye exam and determine if they indicate diabetes. If left untreated, diabetic retinopathy could lead to permanent vision loss
Diabetic Macular Edema
Diabetic retinopathy can eventually advance into diabetic macular edema. This occurs when the retina’s damaged blood vessels leak under the macula, the part of the retina that forms our central vision. The macula can then swell, leading to irreversible damage and vision loss.
Other Diabetic Eye Problems
Diabetes can also increase your risk of other serious eye conditions.
Cataracts
Cataracts are a normal part of aging where our eye’s natural lens hardens and clouds, causing blurry and faded vision. Cataracts mostly affect people over 60, but some factors can increase your risk of developing them early. Diabetes is one of those factors.
People with diabetes are more likely to develop cataracts at an earlier age.
You can manage mild or moderate cataracts with eyeglasses or contacts. Managing blood sugar levels can go a long way in helping to slow the progression of cataracts.
Glaucoma
Glaucoma is a group of eye conditions that cause damage to the optic nerve, usually due to increased pressure in the eye. This can happen when the fluid in the eye cannot drain properly, causing a buildup and damaging the optic nerve fibres. Glaucoma can cause vision loss and, in severe cases, blindness. It’s a serious condition that requires immediate treatment to prevent further damage.
Diabetes can increase your chances of developing some forms of glaucoma.
How to Treat Diabetic Eye Problems
Unfortunately, once the damage is done, it can’t be reversed. However, we can work together to limit diabetes’s progression and manage current symptoms. Getting regular eye exams is vital. The earlier we diagnose diabetic retinopathy or any eye disease, the earlier we can start preventing damage.
We can use diagnostic tools to look beyond what the naked eye can see. Optical coherence tomography (OCT) uses light waves to give us a cross-sectional view of your retina, letting us observe the blood vessels at a new angle. Widefield retinal photography provides us with high-definition images so we can look for abnormalities like hemorrhages or fluids leaking.
If we determine you’re at risk of vision loss from diabetic retinopathy, there are some steps we can take.
The most effective approach is blood sugar control. This involves controlling and monitoring your diet and exercise to keep tight control of your blood sugar levels. This may also include addressing high blood pressure and cholesterol levels since they can also damage the delicate blood vessels.
In some severe cases, you may receive anti-VEGF injections to prevent abnormal blood vessels from growing or laser surgery to seal off leaking blood vessels. However, these only slow or prevent further leaking; they don’t completely reverse the damage.
Early Detection for Early Treatment
If you have diabetes, you should have an eye exam annually. This allows us to detect changes before they become problems. Diabetic eye problems don’t have to be inevitable. Request your appointment at Downtown Vision Care, and let’s prioritize preserving your vision today!